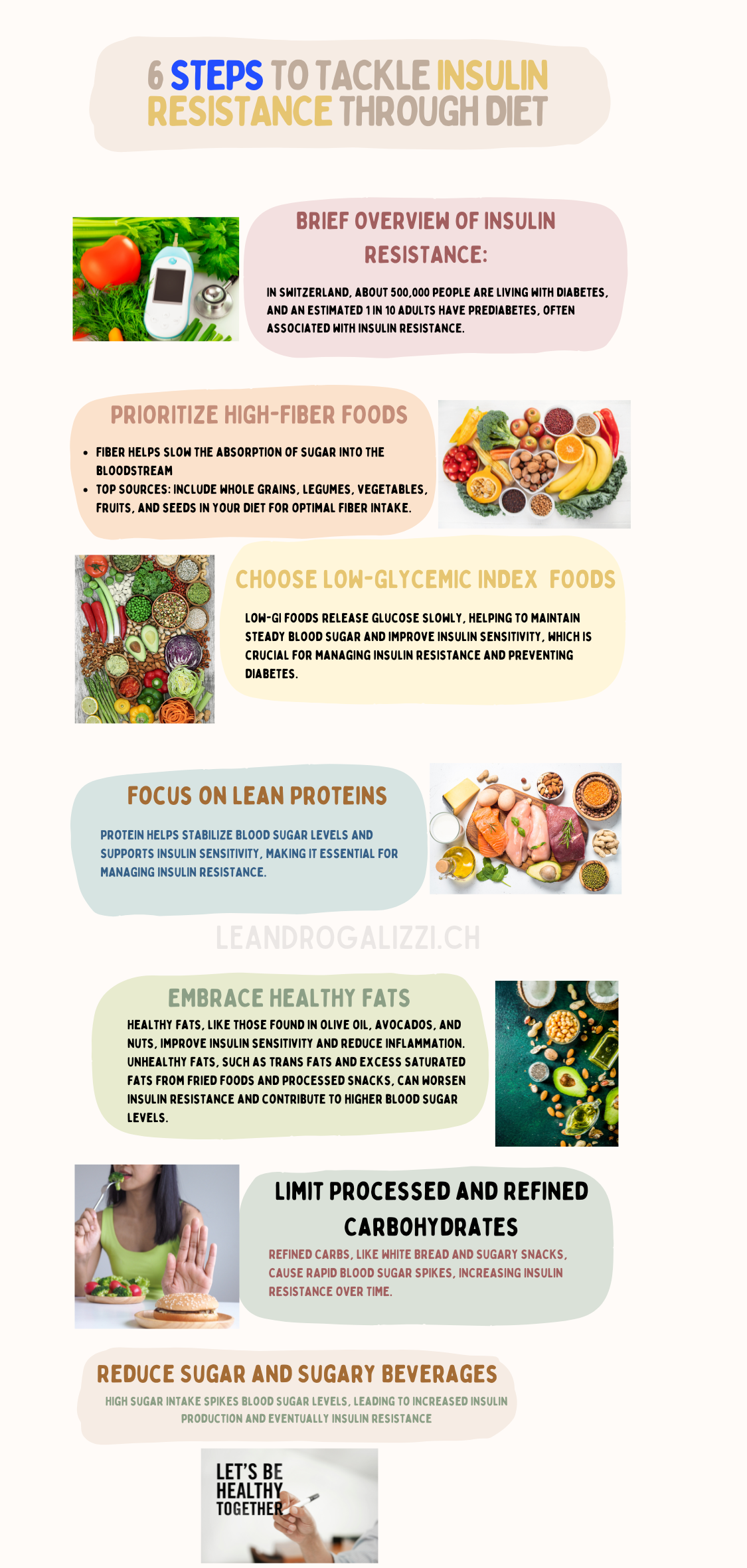
How to Prevent Diabetes: 8 Proven Steps to Tackle Insulin Resistance Through Diet

- Understanding Insulin Resistance
- The Importance of Diet in Preventing Diabetes
- Step 1: Prioritize High-Fiber Foods
- Step 2: Choose Low-Glycemic Index (GI) Foods
- Step 3: Focus on Lean Proteins
- Step 4: Embrace Healthy Fats
- Step 5: Limit Processed and Refined Carbohydrates
- Step 6: Reduce Sugar and Sugary Beverages
- Step 7: Incorporate Antioxidant-Rich Foods
- Step 8: Practice Portion Control and Mindful Eating
- Conclusion
Diabetes is a growing health concern worldwide, with type 2 diabetes making up the majority of cases. One of the primary precursors to type 2 diabetes is insulin resistance, a condition where the body’s cells become less responsive to insulin, making it harder to regulate blood sugar levels. As the prevalence of diabetes continues to rise, especially among adults over 30, the need for effective prevention strategies has never been more urgent.
The good news is that diet plays a crucial role in preventing and managing insulin resistance. By making specific dietary changes, you can significantly reduce your risk of developing type 2 diabetes. In this blog post, we’ll explore eight proven steps you can take to tackle insulin resistance through diet, helping you maintain better health and avoid the complications associated with diabetes.
Understanding Insulin Resistance
What is Insulin Resistance?
Insulin resistance occurs when the cells in your body don’t respond effectively to insulin, a hormone produced by the pancreas that regulates blood sugar levels. When insulin resistance develops, glucose builds up in the blood instead of being absorbed by the cells, leading to higher blood sugar levels. Over time, this can result in prediabetes and eventually type 2 diabetes if not addressed.
Causes and Risk Factors
Several factors contribute to the development of insulin resistance, including poor dietary habits, a sedentary lifestyle, and genetic predisposition. Excess weight, particularly around the abdomen, is one of the most significant risk factors. Understanding these causes can help you take proactive steps to reduce your risk and improve your overall health.
The Importance of Diet in Preventing Diabetes
How Diet Affects Insulin Sensitivity
What you eat has a direct impact on your insulin sensitivity. Certain foods can help stabilize blood sugar levels and improve your body’s ability to use insulin effectively. Conversely, a diet high in processed foods, sugars, and unhealthy fats can exacerbate insulin resistance, making it harder for your body to regulate glucose.
The Benefits of Early Dietary Intervention
Research shows that making dietary changes early on can be incredibly effective in preventing the progression from insulin resistance to diabetes. By focusing on a balanced diet rich in fiber, lean proteins, and healthy fats, you can support your body’s insulin function and reduce the risk of developing diabetes.
Step 1: Prioritize High-Fiber Foods
Why Fiber Matters
Fiber plays a crucial role in managing blood sugar levels and improving insulin sensitivity. High-fiber foods slow down the absorption of sugar into the bloodstream, preventing spikes in blood glucose levels. This not only helps in managing insulin resistance but also contributes to overall digestive health.
Top Fiber-Rich Foods
Incorporating fiber-rich foods into your diet is easier than you might think. Foods like legumes, whole grains, and vegetables are excellent sources of dietary fiber. Examples include beans, lentils, oats, quinoa, and leafy greens like spinach and kale. These foods not only help regulate blood sugar but also keep you feeling fuller for longer, which can aid in weight management.
Tips for Incorporation
To increase your fiber intake, start by adding a serving of high-fiber foods to each meal. For breakfast, consider a bowl of oatmeal topped with fresh berries. At lunch, include a side of lentil soup or a quinoa salad. For dinner, opt for whole grains like brown rice or barley alongside a generous portion of vegetables. By making these simple changes, you can significantly boost your daily fiber intake and improve your insulin sensitivity.
Step 2: Choose Low-Glycemic Index (GI) Foods
Understanding Glycemic Index
The glycemic index (GI) is a system that ranks foods based on how quickly they raise blood sugar levels after consumption. Foods with a high GI cause rapid spikes in blood glucose, while low-GI foods are digested more slowly, leading to a gradual rise in blood sugar. For those managing insulin resistance, choosing low-GI foods can help maintain stable blood sugar levels and improve insulin sensitivity.
Best Low-GI Foods for Insulin Resistance
Incorporating low-GI foods into your diet is a key strategy for managing insulin resistance. Some excellent low-GI options include whole grains like oats and barley, legumes such as lentils and chickpeas, and most fruits and vegetables. Berries, apples, oranges, and non-starchy vegetables like leafy greens and tomatoes are all great choices that provide essential nutrients while helping to keep blood sugar levels in check.
Meal Planning Tips
When planning meals, focus on incorporating a variety of low-GI foods. For breakfast, try a bowl of steel-cut oats topped with a handful of fresh berries. At lunch, enjoy a salad with leafy greens, chickpeas, and a drizzle of olive oil. For dinner, pair lean proteins like grilled chicken or fish with quinoa and steamed vegetables. By consistently choosing low-GI foods, you can help manage insulin resistance and reduce the risk of developing diabetes.
Step 3: Focus on Lean Proteins
The Role of Protein in Blood Sugar Control
Protein plays a vital role in stabilizing blood sugar levels. Unlike carbohydrates, protein has a minimal impact on blood glucose, making it an important component of a diet designed to manage insulin resistance. Eating adequate amounts of protein can also help you feel fuller for longer, which can reduce cravings and prevent overeating.
Healthy Protein Sources
To optimize your diet for insulin sensitivity, focus on lean protein sources. These include options like chicken breast, turkey, fish (especially fatty fish like salmon and mackerel, which are rich in omega-3 fatty acids), tofu, and legumes. Incorporating plant-based proteins, such as beans, lentils, and quinoa, is also beneficial, as they provide fiber and other essential nutrients along with protein.
Incorporating Protein in Every Meal
Aim to include a source of lean protein in every meal. For breakfast, consider eggs or Greek yogurt with a sprinkle of nuts. At lunch, a quinoa salad with grilled chicken or a chickpea wrap can provide a good balance of protein and fiber. For dinner, opt for a serving of fish or tofu with a side of vegetables. These choices help keep blood sugar levels stable throughout the day and support overall health.
Step 4: Embrace Healthy Fats
Good Fats vs. Bad Fats
Not all fats are created equal. While saturated and trans fats can worsen insulin resistance and contribute to heart disease, healthy fats—particularly unsaturated fats—can have the opposite effect. Healthy fats can improve insulin sensitivity, reduce inflammation, and support overall cardiovascular health.
Sources of Healthy Fats
Incorporate sources of healthy fats into your diet to support insulin function. Olive oil, avocados, nuts, seeds, and fatty fish are all excellent options. These foods are rich in monounsaturated and polyunsaturated fats, which are known to help reduce the risk of heart disease and improve insulin sensitivity.
Balancing Fat Intake
While healthy fats are beneficial, it’s important to consume them in moderation. A balanced diet that includes a variety of fat sources is key. For example, use olive oil as a base for salad dressings, add slices of avocado to sandwiches, and include a handful of nuts or seeds as a snack or salad topper. Incorporating fatty fish into your meals at least twice a week can also provide heart-healthy omega-3 fatty acids.
Step 5: Limit Processed and Refined Carbohydrates
The Impact of Processed Foods on Insulin
Processed and refined carbohydrates, such as white bread, pastries, and sugary snacks, can cause rapid spikes in blood sugar, leading to increased insulin production and eventually, insulin resistance. These foods are often stripped of their natural fiber and nutrients, making them less satisfying and more likely to contribute to weight gain and metabolic issues.
What to Avoid
To manage insulin resistance effectively, it’s important to limit foods that are high in refined carbohydrates. This includes white bread, white rice, sugary cereals, pastries, and most packaged snacks. These foods can cause significant fluctuations in blood sugar levels, which can strain your body’s ability to produce and use insulin effectively.
Healthier Alternatives
Instead of processed and refined carbohydrates, opt for whole grains and other unprocessed options. Replace white bread with whole-grain or sprouted bread, choose brown rice or quinoa over white rice, and snack on whole fruits, nuts, or seeds instead of sugary treats. By making these simple swaps, you can maintain more stable blood sugar levels and reduce your risk of insulin resistance.
Step 6: Reduce Sugar and Sugary Beverages
Sugar’s Role in Insulin Resistance
High sugar intake is a major contributor to insulin resistance. When you consume sugary foods and beverages, your blood sugar levels spike, prompting your body to release large amounts of insulin. Over time, this can lead to insulin resistance, where your cells become less responsive to insulin, increasing the risk of developing type 2 diabetes.
Alternatives to Sugary Drinks
Sugary beverages, such as sodas, fruit juices, and sweetened teas, are some of the biggest culprits when it comes to insulin resistance. Replacing these with healthier alternatives can have a significant impact on your health. Opt for water, sparkling water with a splash of lemon or lime, herbal teas, or black coffee. These choices can help you stay hydrated without adding unnecessary sugar to your diet.
Tips for Reducing Sugar in Your Diet
Reducing your sugar intake doesn’t have to be difficult. Start by cutting back on obvious sources like sugary snacks and desserts. Read food labels carefully to spot hidden sugars in products like sauces, dressings, and packaged foods. Gradually reduce the amount of sugar you add to coffee or tea, and try using natural sweeteners like stevia or monk fruit if you need a sweet fix. Over time, your taste buds will adjust, and you’ll find you crave less sugar overall.
Step 7: Incorporate Antioxidant-Rich Foods
Why Antioxidants Matter
Antioxidants are compounds that help fight inflammation and oxidative stress, both of which are linked to insulin resistance. By including more antioxidant-rich foods in your diet, you can support your body’s ability to manage blood sugar and improve overall health.
Top Antioxidant Foods
Some of the best sources of antioxidants include colorful fruits and vegetables like berries, spinach, kale, and bell peppers. Nuts, seeds, and dark chocolate also provide a good dose of antioxidants. Incorporating a variety of these foods into your daily meals can help combat the inflammation associated with insulin resistance.
Daily Incorporation Tips
Adding antioxidant-rich foods to your diet is simple and delicious. Start your day with a smoothie made from spinach, berries, and a scoop of protein powder. Add a handful of nuts or seeds to your salads or yogurt for a crunchy, nutrient-rich boost. When cooking, include a variety of colorful vegetables, and consider using herbs and spices like turmeric and ginger, which also have powerful antioxidant properties.
Step 8: Practice Portion Control and Mindful Eating
The Importance of Portion Control
Even the healthiest foods can contribute to weight gain and insulin resistance if eaten in large quantities. Portion control is crucial for maintaining a healthy weight and ensuring that your body can effectively manage blood sugar levels. Eating appropriate portions helps prevent overeating and reduces the likelihood of insulin resistance.
Mindful Eating Practices
Mindful eating involves paying attention to your hunger and fullness cues and savoring each bite of your meal. This practice can help you avoid overeating and make healthier food choices. By eating slowly and without distractions, you’re more likely to notice when you’re satisfied, which can prevent overindulgence and support better blood sugar control.
Practical Portion Control Tips
To practice portion control, try using smaller plates and serving sizes. Start with a modest portion, and if you’re still hungry after eating, wait 10-15 minutes before deciding whether to have more. This gives your body time to register fullness. Additionally, avoid eating directly from large packages or containers, which can make it difficult to gauge how much you’re consuming. Instead, portion out your snacks into smaller bowls or plates.
Conclusion
Managing insulin resistance is a crucial step in preventing type 2 diabetes, and diet plays a central role in this process. By prioritizing high-fiber foods, choosing low-glycemic index options, focusing on lean proteins, embracing healthy fats, limiting processed carbohydrates, reducing sugar intake, incorporating antioxidant-rich foods, and practicing portion control, you can significantly improve your insulin sensitivity and lower your risk of diabetes.
These dietary changes are not just about preventing disease—they’re about enhancing your overall health and well-being. By making small, consistent changes to your diet, you can create a sustainable, healthy lifestyle that supports your body’s natural ability to regulate blood sugar. Start implementing these steps today, and take control of your health for the long term.
Learn more about the impact of sugar on insulin resistance from the American Diabetes Association
References
- Centers for Disease Control and Prevention. Candidiasis. Accessed 6/6/2022.
- Edwards, Jr. JE. Candidiasis. Harrison’s Principles of Internal Medicine, 20e. New York: McGraw Hill; 2018. Accessed 6/6/2022.
- Merck Manual. Candidiasis. Accessed 6/6/2022.
- National Organization for Rare Disorders. Candidiasis. Accessed 6/6/2022.
- StatPearls. Candidiasis. Accessed 6/6/2022.
- U.S. Department of Health and Human Services. Vaginal Yeast Infections. Accessed 6/6/2022.
- Noble, S. M. Candida albicans cell type switches and functional plasticity in the mammalian host. PubMed Central. 2016.
- Agarwal, S. Assessment and clinical interpretation of reduced IgG values. NCBI. 2007.
- Tefferi, A. How to Interpret and Pursue an Abnormal Complete Blood Cell Count in Adults. Mayo Clinic Proceedings. 2005.
- Christensson, B., Sigmundsdottir, G., & Larsson, L. D-arabinitol–a marker for invasive candidiasis. PubMed. 1999.





